Dieter Egli was just about to start graduate school in 1998 when researchers first worked out how to derive human embryonic stem cells. In the two decades since, the prolific cells have been a fixture of his career. The biologist, now at Columbia University in New York City, has used them to explore how DNA from adult cells can be reprogrammed to an embryonic state, and to tackle questions about the development and treatment of diabetes. He has even helped to develop an entirely new form of human embryonic stem cell that could simplify studies on what different human genes do1.
His wide-ranging research established him as a leader in embryonic stem-cell biology, a field challenged by restricted funding and an enthusiasm for competing technologies that don’t carry the same ethical baggage. Still, many say that human embryonic stem cells are now more relevant than ever. “I am very excited about embryonic stem cells,” says Egli. “They will lead to unprecedented discoveries that will transform life. I have no doubt about it.”
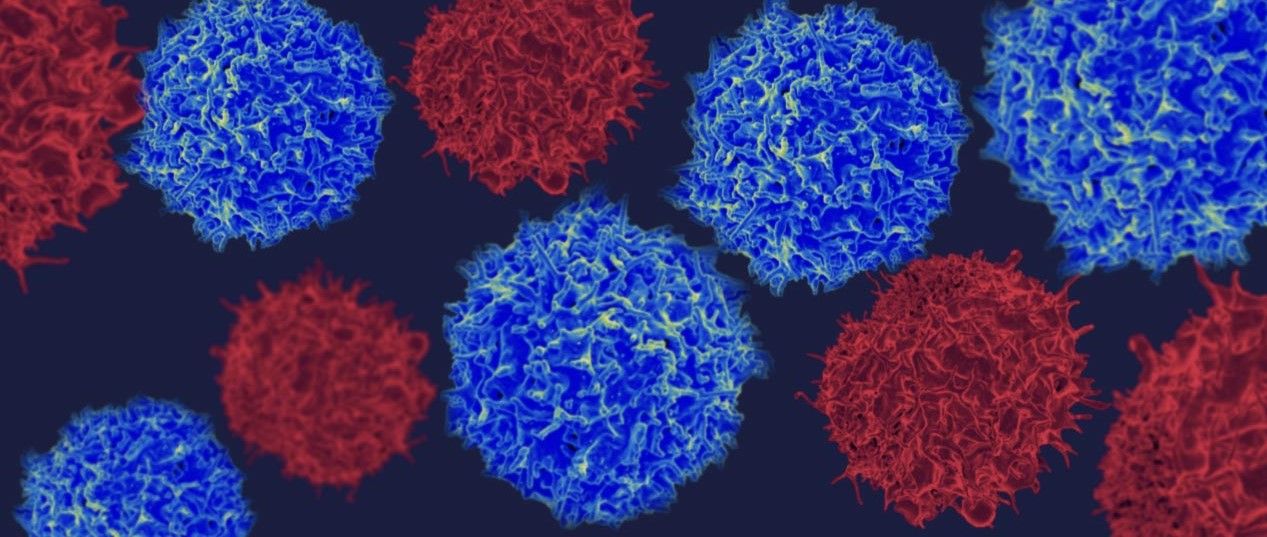
Embryonic stem (ES) cells provide unparallelled information on early development. Like astronomers looking back to the Big Bang for fundamental insight about the Universe, biologists rake over the molecules inside these remarkable entities for clues as to how a single original cell turns into trillions, with a dizzying array of forms and functions. Scientists have learnt how to turn the cells into dozens of mature cell types representing various tissues and organs in the body. These are used to test drugs, to model disease and, increasingly, as therapies injected into the body. Starting with an attempt to repair spinal-cord injuries in 2010, there have been more than a dozen clinical trials of cells created from ES cells — to treat Parkinson’s disease and diabetes, among other conditions. Early results suggest that some approaches are working: a long-awaited report this week shows improved vision in two people with age-related macular degeneration, a disease that destroys the sharpness of vision2.
“In some ways, it’s not a surprise, because 20 years ago we expected it,” says Egli, “but I’m still surprised that this promise is becoming a reality.”
Researchers also discussed plans to derive stem cells from embryos made by a process called somatic-cell nuclear transfer — the same method used to create cloned animals such as Dolly the sheep — in which the nucleus from an adult donor cell is transferred into a human egg that has had its nucleus removed. The rationale for this ‘therapeutic cloning’ was to provide a limitless source of dynamic cells with the same DNA as the cell donor. They started talking about studying complex genetic diseases ‘in a dish’ and replacing failing organs and tissues in the same the way that mechanics replace car parts. There were several false starts, notably in 2005, when investigators found that South Korean scientist Woo Suk Hwang had fraudulently claimed to have isolated stem cells in this way. But by 2013, a team led by Shoukhrat Mitalipov, a stem-cell researcher at the Oregon Health and Science University in Portland, finally succeeded8.
Researchers are also trying to grow organs. Given the right signalling molecules and 3D environment, ES cells organize into complex tissues known as organoids, even in a dish. This capacity is important for researchers such as James Wells at Cincinnati Children’s Hospital in Ohio, who is developing intestinal organoids for testing drugs, and perhaps one day for transplant.
And new sources of ES cells have presented other research tools for genetic disease. In 2004, for example, fertility doctors in Chicago started making ES-cell lines from embryos created through in vitro fertilization that had been found to have a genetic defect, and thus were rejected for fertility treatments. This allowed the team to create cellular models of thalassaemia, Huntington’s disease, Marfan’s syndrome, muscular dystrophy and other genetic conditions13. In 2007, researchers used ES cells to pin down the molecular changes that lead to cognitive impairments seen in a heritable condition known as Fragile X syndrome14.
Pathway to promise
ES-cell research still has room to grow, if it can get past some hurdles. One big problem is that many cell types are challenging to produce. Melton estimates that only about ten cell types created so far are truly functional equivalents of normal human cells. And some with the most far-reaching uses, such as eggs and sperm, are expected to remain a challenge for the foreseeable future.
The field also faces uncertainty about funding. Scientists have heard frequent rumours that US president Donald Trump might impose new restrictions on federal funding for research on ES cells.
But despite their sometimes rocky history, ES cells have proved their value repeatedly, and in some unpredictable ways, say many investigators. Some researchers have even scaled back their use of animal models because ES cells seem to provide a better path to studying human disease. “My motto was, ‘all human, all the time’,” Melton says.
Yamanaka says that ES cells were the motivation for his own work on iPS cells. And it was Thomson’s recipe for human ES cells that allowed the shift from mouse to human iPS cells in just one year, after it had taken nearly two decades to move from mouse ES cells to the human variety. “We knew exactly how we should culture human iPS cells,” says Yamanaka.
ES cells are just as crucial today, he says, for better understanding the mechanism of pluripotency and for improving the medical application of any pluripotent cell. “The importance of human ES cells is no less now than 20 years ago, and I do not imagine it will be any lower in the future,” he says.